Disease of the Month – Gastroparesis
Shots:
-
Gastroparesis is a chronic gastrointestinal disorder characterized by delayed gastric emptying, leading to symptoms such as nausea, vomiting, bloating, and early satiety. This condition significantly affects patients' quality of life, posing challenges for diagnosis and treatment.
-
Our Disease of the Month report covers epidemiology, market size, current management strategies, emerging therapeutic options, and the role of patient advocacy groups. Additionally, we highlight the key industry players advancing treatment for gastroparesis.
-
For a detailed analysis and tailored insights into the gastroparesis landscape, contact our experts at connect@pharmashots.com.

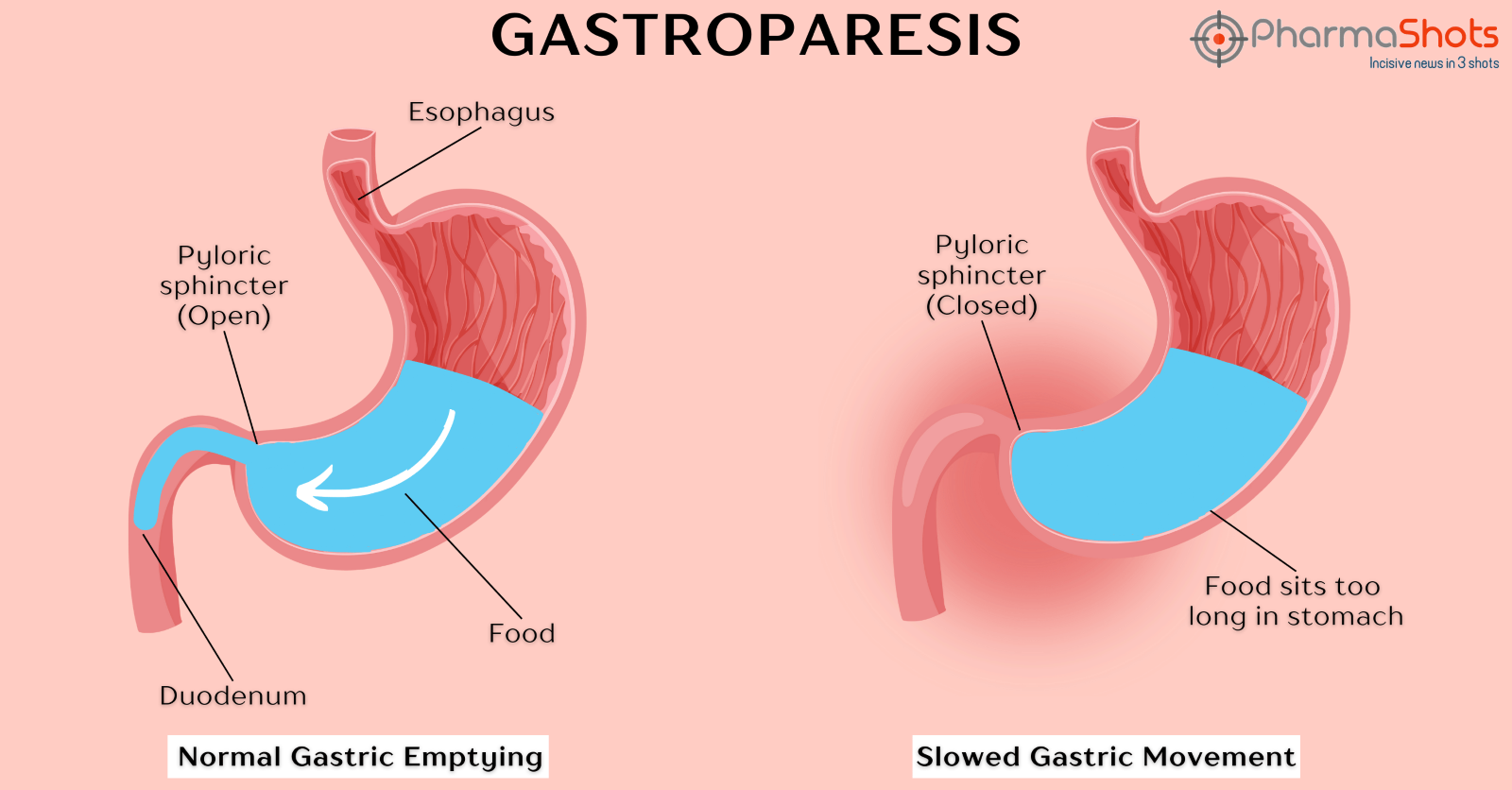
Gastroparesis, often described as a paralysis of the stomach, is a functional disorder in which the stomach's ability to empty its contents is impaired. It affects the nerves and muscles of the stomach, resulting in weaker and slower peristalsis than needed for proper digestion. Consequently, food remains in the stomach longer than normal, sometimes forming a hardened mass known as a bezoar. [1]
 Common symptoms of gastroparesis include: [1,2]
Common symptoms of gastroparesis include: [1,2]
-
Feeling of fullness
-
Bloating
-
Nausea and vomiting
-
Regurgitation of undigested food
-
Anorexia
-
Abdominal pain
-
Acid reflux and heartburn
-
Indigestion
-
Blood sugar fluctuations
-
Constipation

Gastroparesis can be categorized based on its underlying cause: [1]
-
Diabetic gastroparesis: Resulting from uncontrolled diabetes
-
Post-surgical gastroparesis: Due to complications following surgery
-
Idiopathic gastroparesis: With no identifiable cause
The major cause of gastroparesis is nerve impairment in the stomach muscles that control muscle contractions and gastric emptying. Other known causes include: [1,3]
- Diabetes: Hyperglycemia damages the vagus nerve and pacemaker cells, causing delayed gastric emptying.
- Surgery: Surgical procedures near the stomach can damage the vagus nerve, leading to gastroparesis. Procedures that may cause this include:
- Nissen fundoplication
- Gastrectomy
- Gastric bypass surgery
- Pancreatectomy
- Vagotomy
- Cholecystectomy
- Infections: Gastrointestinal infections such as norovirus or rotavirus can cause gastroparesis.
- Autoimmune diseases: Disorders like lupus or scleroderma can lead to gastroparesis.
- Drugs: Medications like narcotics, anticholinergics, calcium channel blockers, and others can interfere with nerve signals, resulting in gastroparesis.
- Other causes: Less common causes include:
- Neurological diseases: Conditions like Parkinson's disease, multiple sclerosis, or autonomic dysfunction
- Collagen vascular diseases: Diseases such as amyloidosis, scleroderma, or Ehlers-Danlos syndrome
- Endocrine diseases: Conditions like thyroid disease, adrenal disorders, or electrolyte imbalances
- Cystic fibrosis: Resulting in mucus accumulation in the gastrointestinal tract
 Gastroparesis is diagnosed through a combination of clinical evaluation, medical history, and specialized tests to assess gastric emptying. Common diagnostic methods include: [2,3]
Gastroparesis is diagnosed through a combination of clinical evaluation, medical history, and specialized tests to assess gastric emptying. Common diagnostic methods include: [2,3]
-
Upper Gastrointestinal Barium Contrast Radiography: Swallowing a barium solution to detect abnormalities
-
Upper Endoscopy: Visualizing the esophagus, stomach, and duodenum for obstructions
-
Gastric Emptying Scintigraphy: Using a radiolabeled meal to monitor gastric emptying
-
Antroduodenal Manometry: Using a catheter to measure electrical and muscular activity
-
Wireless Motility Study: Ingesting a small pill to collect gastrointestinal data

Effective management of gastroparesis requires accurate diagnosis to address the underlying causes. Treatment options include: [2,4]
-
Dietary changes: Switching to a liquid diet, consuming small and frequent meals, following a low-fat, low-fiber diet, and avoiding high-sugar foods
-
Medications: Prokinetics (e.g., erythromycin, metoclopramide) and anti-emetics for symptom relief
-
Endoscopic therapy: For cases unresponsive to dietary or medical management
-
Experimental therapies:
-
Gastric electric stimulation (gastric pacing) to stimulate muscle movement
-
Botulinum toxin injections to reduce gastric muscle spasms
-
Endoscopic pyloromyotomy and other surgical interventions in rare cases

-
Prevalence: In the US adult population, the prevalence of gastroparesis is estimated to range from 13.8 to 267.7 cases per 100,000 individuals. [5]
-
Incidence: The incidence of gastroparesis is estimated to range from 1.9 to 6.3 cases per 100,000 person-years. [5]
-
Gender: The incidence of gastroparesis in women is four times higher than that of men (4:1). [6]
-
Etiology: The leading causes of gastroparesis include diabetes (57.4%), postsurgical complications (15.0%), drug-induced cases (11.8%), and idiopathic origins (11.3%). [7]
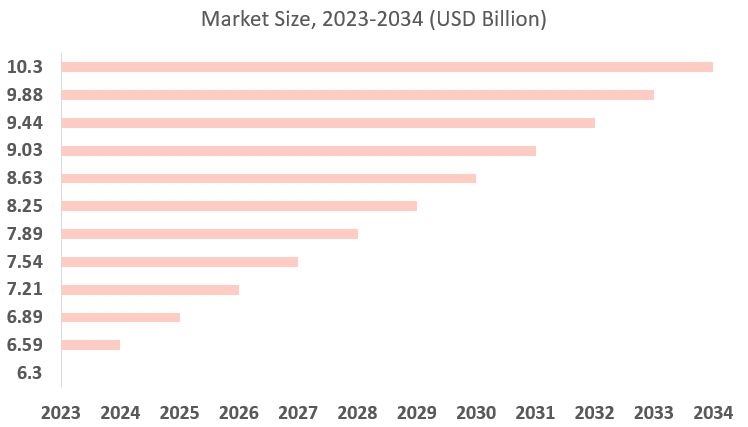
 The global market for gastroparesis treatment was valued at $6.3 billion in 2023 and is projected to reach $10.3 billion by 2034, with a CAGR of 4.6% from 2024 to 2034. [8]
The global market for gastroparesis treatment was valued at $6.3 billion in 2023 and is projected to reach $10.3 billion by 2034, with a CAGR of 4.6% from 2024 to 2034. [8]
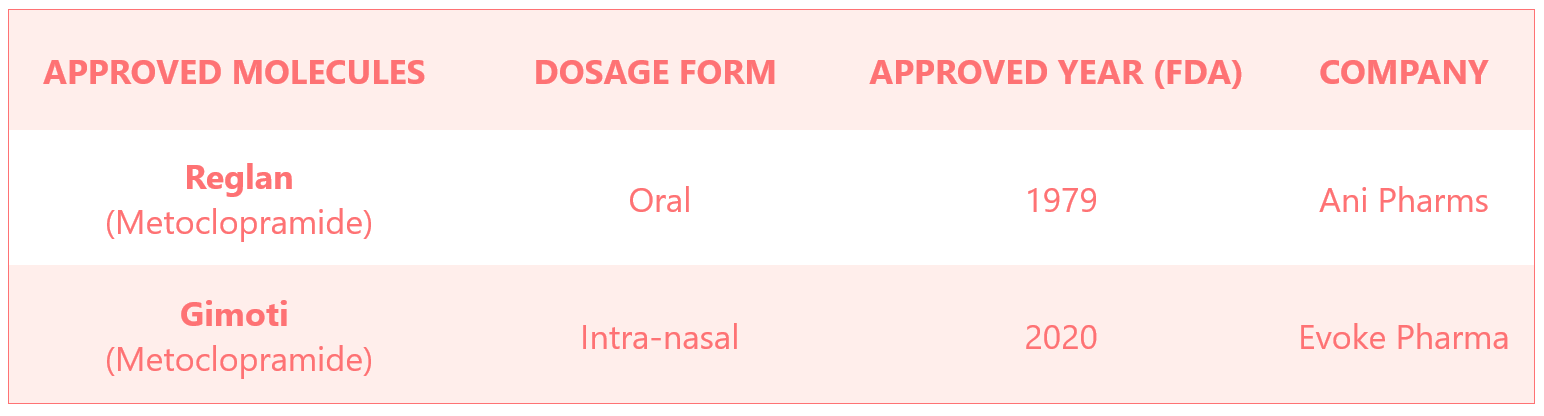
 Gimoti is the first and only nasally administered product indicated for the relief of symptoms in adults with acute and recurrent diabetic gastroparesis. Reglan as an oral formulation was already approved to treat gastroparesis in 1979, whereas Gimoti was approved as an intranasal formulation of metoclopramide in 2020.
Gimoti is the first and only nasally administered product indicated for the relief of symptoms in adults with acute and recurrent diabetic gastroparesis. Reglan as an oral formulation was already approved to treat gastroparesis in 1979, whereas Gimoti was approved as an intranasal formulation of metoclopramide in 2020.
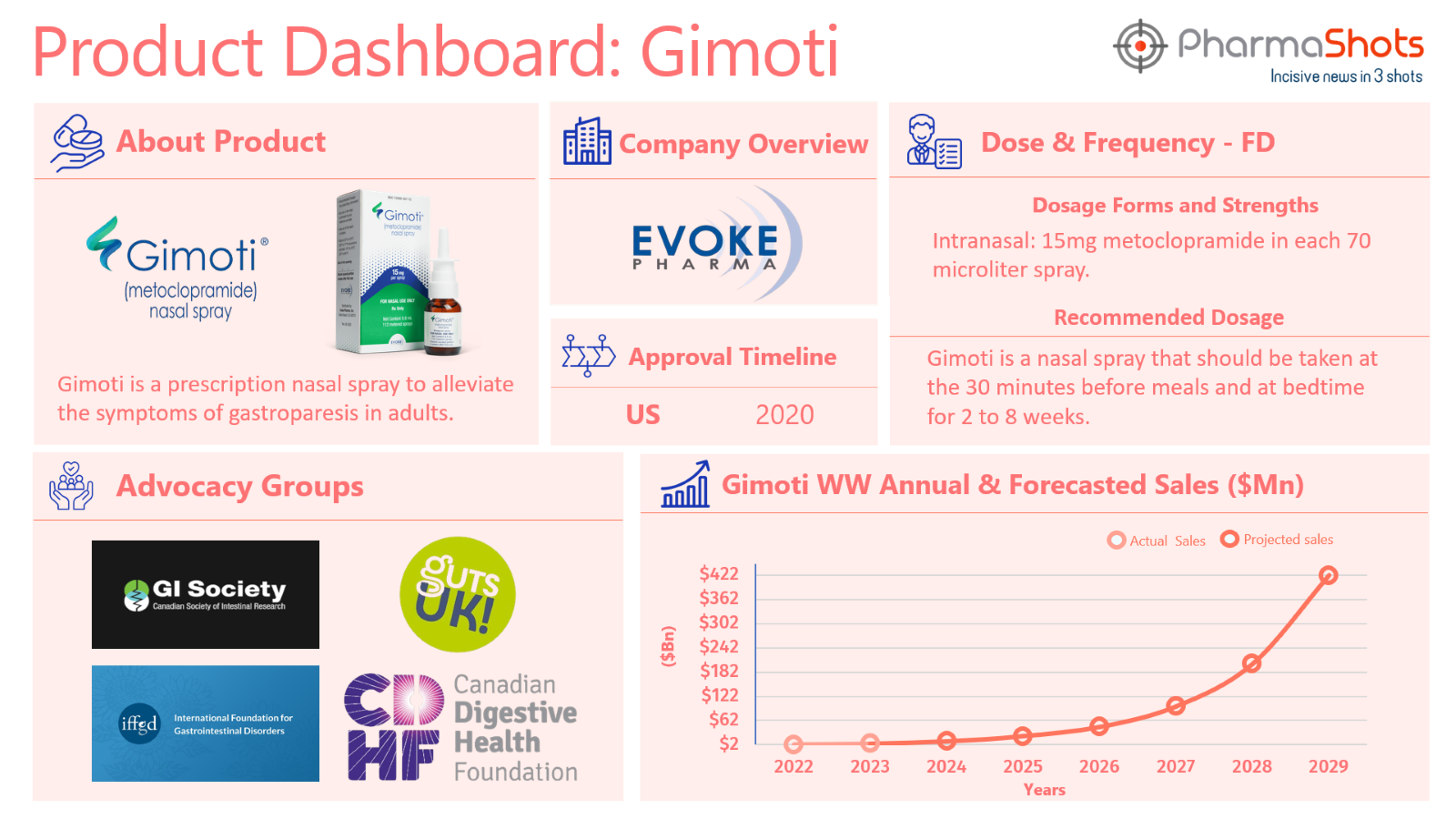
 The approved treatments for gastroparesis include Reglan (oral formulation) by Ani Pharmaceuticals and Gimoti (intranasal formulation) by Evoke Pharma.
The approved treatments for gastroparesis include Reglan (oral formulation) by Ani Pharmaceuticals and Gimoti (intranasal formulation) by Evoke Pharma.
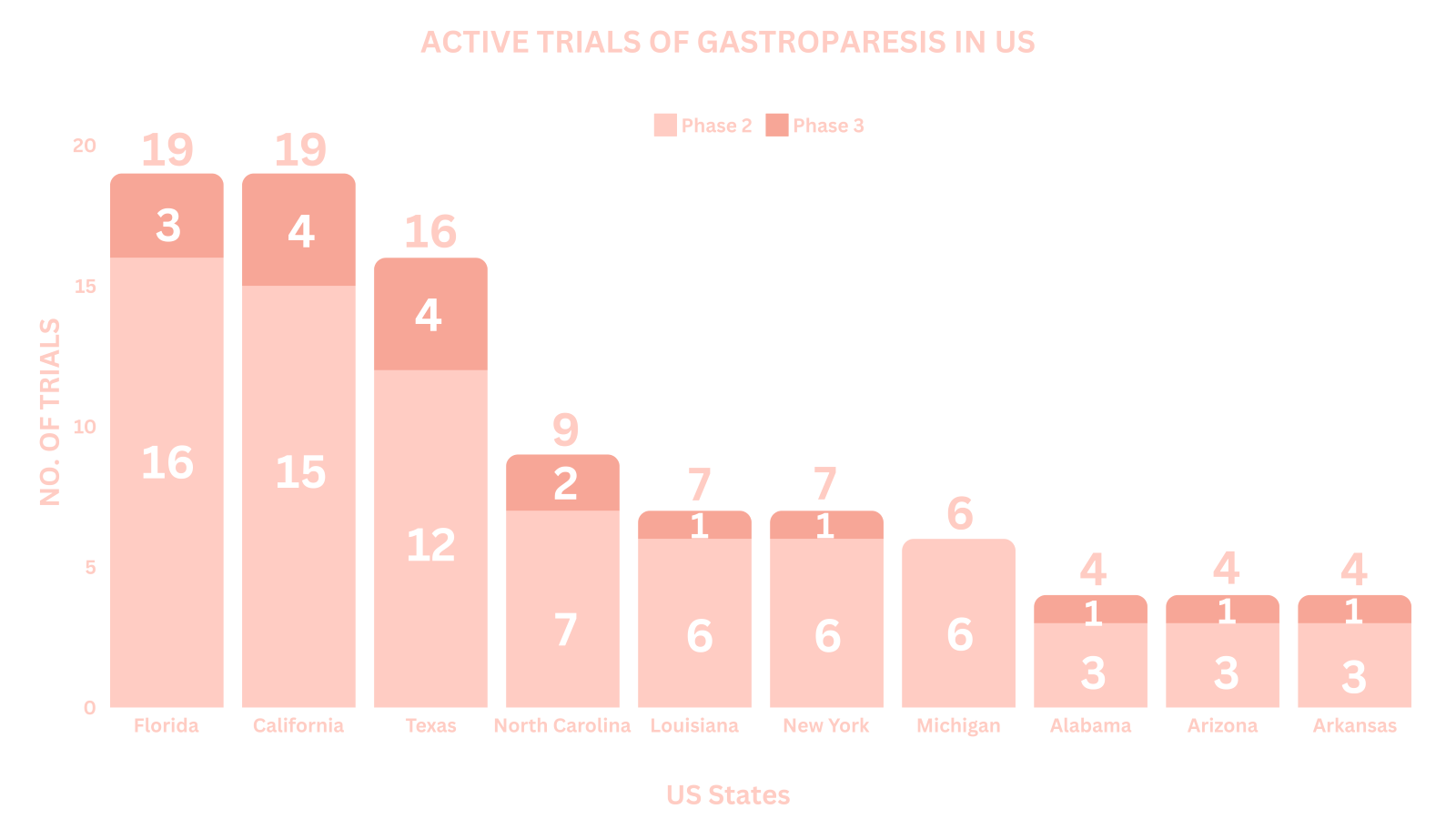
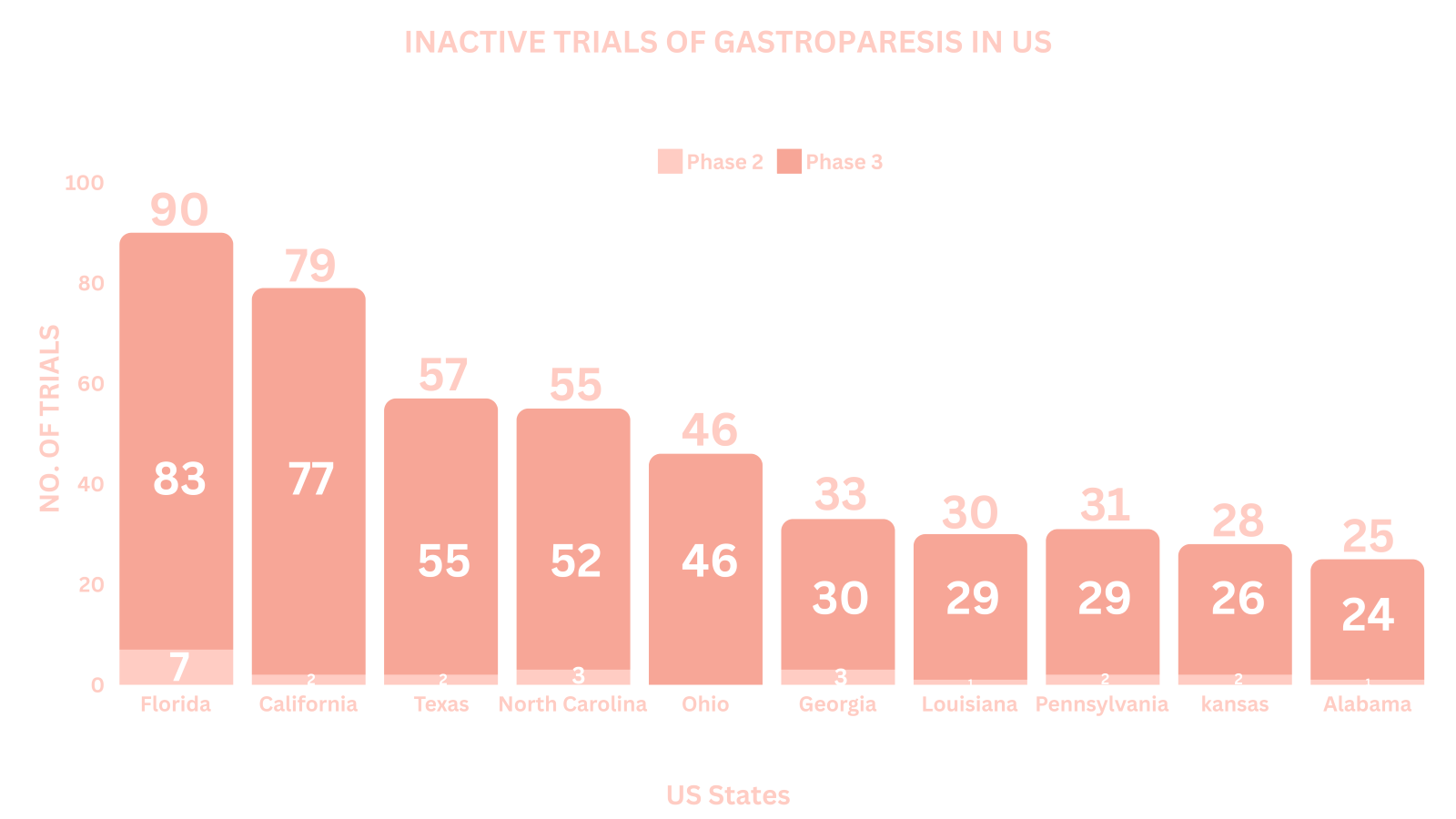
 Based on the geographical distribution, the interventional and industry-sponsored clinical trials are classified in the below-mentioned graph into two groups based on their status: Active (recruiting; active, not recruiting; not yet recruiting; enrolling by invitation and suspended) and Inactive (withdrawn; terminated and trials with unknown status)
Based on the geographical distribution, the interventional and industry-sponsored clinical trials are classified in the below-mentioned graph into two groups based on their status: Active (recruiting; active, not recruiting; not yet recruiting; enrolling by invitation and suspended) and Inactive (withdrawn; terminated and trials with unknown status)
The maximum number of active trials is being conducted across the different US states (as represented in the graph) [9]
Note: The number of trials were extracted on Nov 06, 2024.
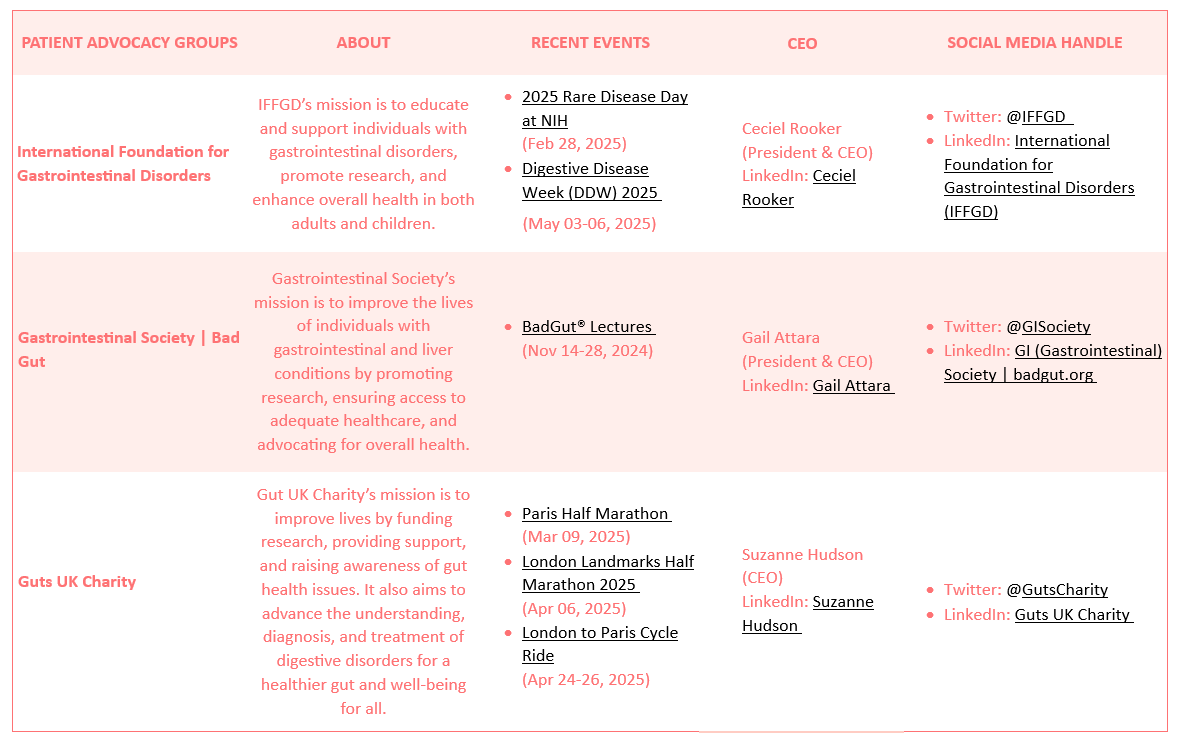
 Several patient advocacy groups are dedicated to supporting individuals with gastroparesis and improving their quality of life.
Several patient advocacy groups are dedicated to supporting individuals with gastroparesis and improving their quality of life.

-
Rachel’s Story
I’m Rachel and I’m 35. I live in West Sussex and work as an executive assistant in nursing. I have worked in healthcare for over 18 years. I have a son, Vinnie, who is nearly five years old. He has autism and knows about my condition. I believe in raising him to be educated about all our differences as people, including health conditions. He knows that sometimes, for example, Mummy can’t eat like him because of gastroparesis. “It took me four years to get a diagnosis, all in all. When I finally received my gastroparesis diagnosis, I felt mixed emotions. On one hand, I felt such a relief to know that four years of trying to convince doctors that my daily “normal” wasn’t right, in just ten-minute appointment slots, had paid off. I finally felt heard. On the other hand, I felt a wave of sadness. I knew my life would never be the same. Over time, I had to process grief. Grief for the healthy body I once knew but was now a long-lost friend. [10]
-
Tonya’s Story
Hello. It took me a while to get my official Gastroparesis diagnosis. My symptoms started in the military. While serving though, I was told such things as it is viral, IBS, or constipation.
Many years later, through the VA, I was finally diagnosed with Gastroparesis based on symptoms and a Gastric Emptying Study. I was given Reglan and told that is all that the VA could do for me.
I requested to go elsewhere for care. As I knew that there were other treatments out there. I had to go over 4 hrs away to Houston for treatment. There I ended up getting a gastric stimulator and then a jejunal feeding tube (into the small intestine). This only worked temporarily for me.
I moved my care and was put on TPN (total parental nutrition). This has been the best treatment for me so far.
I have since been diagnosed with Autonomic Dysfunction and specifically Autoimmune Autonomic Gangliopathy. This contributes to my Gastroparesis, Hypotension, Hypoglycemia, Colonic Dysmotility, Dysphagia, and other bodily systems.
All in all, I am thankful for the diagnoses as I know what is causing these symptoms and can better care for myself.
I also advocate for my care and others now. I have also become an Oley Ambassador, which I enjoy so much. [11]
References
- Cleveland Clinic
- Hopkins Medicine
- NIDDK (NIH)
- Mayo Clinic
- NCBI
- Uptodate
- Gastrojournal
- Globenewswire
- ClinicalTrials.gov
- GutsCharity.org
- IFFGD.org
Related Post: Disease of the Month – Psoriatic arthritis
Tags

A passionate content writer with expertise in delivering high-quality and engaging content, Dipanshu is a keen reader and a versatile writer. Dipanshu dedicatedly covers news ranging from biopharma, life sciences, biotech, and MedTech to diagnostics and animal health companies, FDA, EMA, and biosimilar approvals. He can be contacted at connect@pharmashots.com